Understanding Degenerative Disc Disease Of The Lumbar Spine ICD 10: A Deep Dive
Listen up, folks—Degenerative Disc Disease (DDD) of the lumbar spine is no joke. It's one of those conditions that can creep up on you, leaving you in pain and wondering what went wrong. If you've been hearing about the "ICD 10" code for this issue, you're not alone. Let's break it down, shall we? Whether you're a patient trying to understand your diagnosis or a healthcare professional brushing up on the latest info, this article's got you covered.
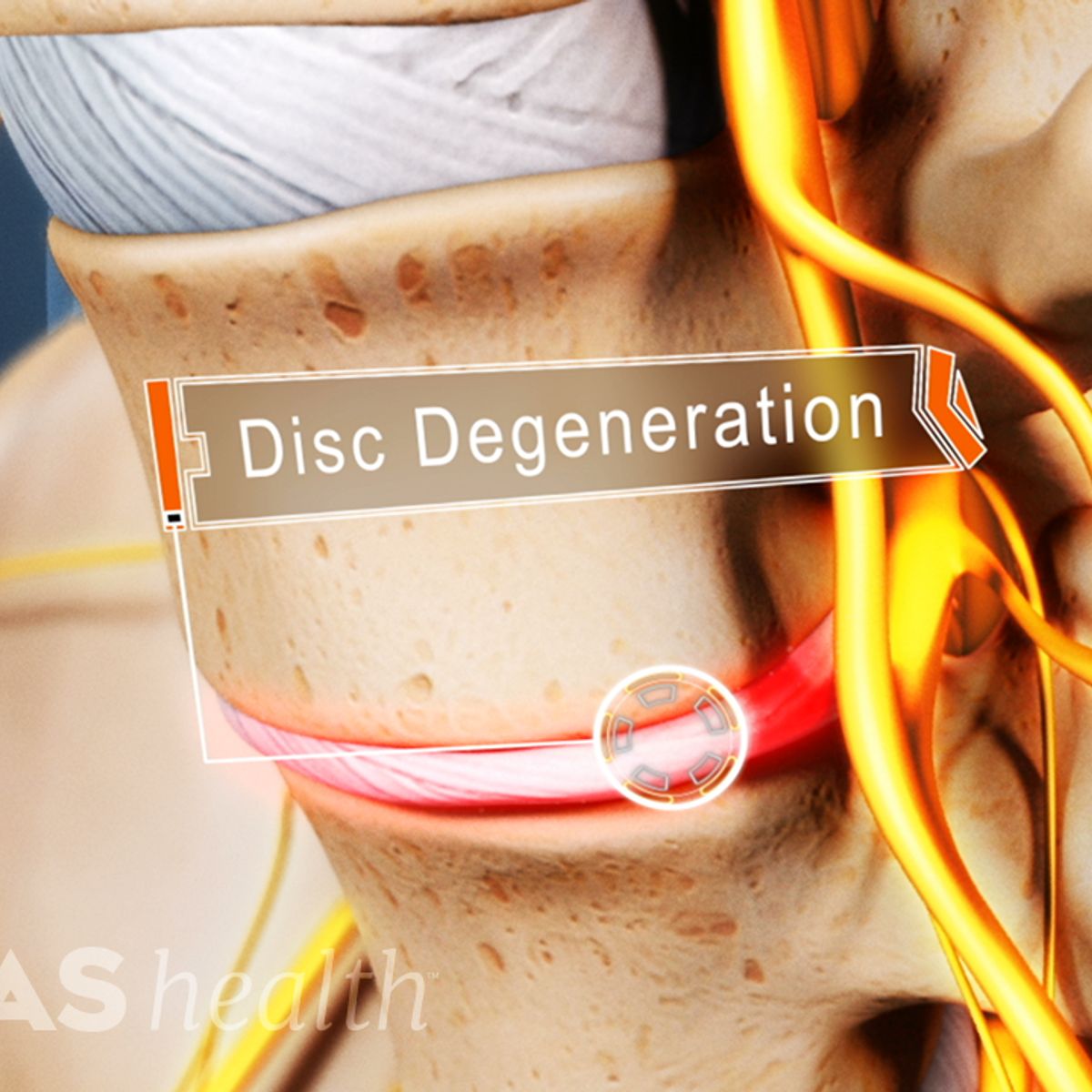
Now, before we dive headfirst into the nitty-gritty, let’s set the scene. Degenerative Disc Disease isn’t actually a disease—it’s more like a condition that happens when the discs in your spine start to break down over time. And when we’re talking about the lumbar spine, well, that’s the lower back area where a lot of the action happens. It’s like the foundation of your body, so when it starts to act up, you feel it big time.
So why does the ICD 10 code matter? Well, it’s the language doctors and insurance companies use to classify and communicate about health conditions. Think of it as the secret code that helps ensure everyone’s on the same page when it comes to diagnosis and treatment. Ready to learn more? Let’s get started!
- Movierulz Kannada Movies Find Legal Streaming Options More
- Noelle Leyva The Truth Behind The Leaks Amp Her Rise
What Exactly is Degenerative Disc Disease of the Lumbar Spine?
Alright, let’s talk about the basics. Degenerative Disc Disease of the lumbar spine is basically what happens when the discs in your lower back start to wear out. These discs act like cushions between the bones in your spine, and when they break down, they can cause a whole lot of trouble. Picture it like this: imagine your spine as a stack of blocks, and the discs are the padding between them. Over time, that padding can flatten, crack, or even dry out, leading to pain, stiffness, and other not-so-fun symptoms.
Here’s the kicker: DDD isn’t something that happens overnight. It’s usually a gradual process that occurs with age, but it can also be sped up by factors like injury, poor posture, or repetitive strain. And when it affects the lumbar spine, it can really mess with your quality of life. Simple things like bending over or lifting something heavy can become major challenges.
Common Symptoms to Watch Out For
Let’s talk about the signs that might indicate you’re dealing with DDD in your lumbar spine. Here’s a quick rundown:
- 7movierulz Kannada Movies 2024 What You Need To Know
- Vegamovies Watch Bollywood More Is It Legal Find Alternatives
- Chronic lower back pain that comes and goes
- Pain that gets worse with sitting, bending, or lifting
- Stiffness in the lower back, especially in the morning
- Pain that radiates to the hips, buttocks, or legs
- Numbness or tingling in the legs (in more severe cases)
Now, these symptoms can vary from person to person. Some folks might experience mild discomfort, while others could be dealing with debilitating pain. It all depends on the severity of the condition and how much the discs have degenerated.
ICD 10 Codes: The Language of Diagnosis
So, what’s the deal with ICD 10 codes? Well, they’re basically a standardized system used worldwide to classify medical conditions. For Degenerative Disc Disease of the lumbar spine, the ICD 10 code you’ll often see is M50.3. But here’s the thing: there are variations depending on the specific location and severity of the condition. For example:
- M50.3 – Cervical disc degeneration
- M51.0 – Lumbar disc degeneration
- M51.2 – Thoracic disc degeneration
These codes help doctors communicate clearly with each other and with insurance companies. They also play a big role in research and tracking trends in healthcare. So if you ever see these codes on your medical records, now you know what they mean!
Why ICD 10 Codes Matter for Patients
For patients, understanding ICD 10 codes can be super helpful. It gives you a clearer picture of your diagnosis and can make navigating the healthcare system a little less confusing. Plus, if you ever need to explain your condition to someone else—whether it’s a doctor, a physical therapist, or even a family member—having the right code can make all the difference.
And let’s not forget about insurance. Insurance companies rely heavily on ICD 10 codes to determine coverage and reimbursement. So if your doctor uses the wrong code, it could mean delays in getting the treatment you need. That’s why it’s always a good idea to double-check and make sure everything’s accurate.
Causes and Risk Factors
Now, let’s talk about what causes Degenerative Disc Disease of the lumbar spine. As we mentioned earlier, aging is a big factor. As we get older, the discs in our spine naturally lose water content, making them less flexible and more prone to damage. But there are other factors at play too:
- Repetitive strain or injury to the back
- Poor posture over time
- Smoking (yep, it affects your spine too!)
- Obesity or being overweight
- Genetics (some people are just more prone to DDD)
It’s important to note that while some of these factors are out of our control, others—like posture and weight management—are things we can work on to reduce our risk. Prevention is key, folks!
How Aging Affects the Spine
Let’s zoom in on how aging impacts the spine. As we grow older, the discs in our spine lose height and elasticity. This can lead to narrowing of the spaces between the vertebrae, which puts more pressure on the nerves. Think of it like a car tire losing air pressure—things just don’t function as smoothly as they used to. And when that happens in your spine, it can lead to pain and other complications.
But here’s the good news: just because you’re getting older doesn’t mean you’re destined to suffer from DDD. There are plenty of things you can do to keep your spine healthy and strong, even as the years go by. We’ll talk more about that later!
Diagnosing Degenerative Disc Disease
So, how do doctors diagnose Degenerative Disc Disease of the lumbar spine? It usually starts with a thorough medical history and physical exam. Your doctor will ask about your symptoms, when they started, and what makes them better or worse. They’ll also check for areas of tenderness, stiffness, and range of motion.
In some cases, imaging tests like X-rays, MRIs, or CT scans may be necessary to get a clearer picture of what’s going on inside your spine. These tests can help identify things like disc degeneration, bone spurs, or nerve compression. And while they might sound intimidating, they’re actually pretty routine and can provide valuable insights into your condition.
What to Expect During a Physical Exam
During a physical exam for DDD, your doctor might do things like:
- Check your reflexes
- Test your muscle strength
- Assess your range of motion
- Look for areas of tenderness or swelling
It’s important to be honest and detailed when describing your symptoms. The more information you can provide, the better equipped your doctor will be to make an accurate diagnosis. And don’t be afraid to ask questions—if something doesn’t make sense, speak up!
Treatment Options for DDD
Alright, let’s talk about the good stuff—treatment options. The good news is that there are plenty of ways to manage Degenerative Disc Disease of the lumbar spine. The key is finding the right combination of treatments that work for you. Here are some common approaches:
- Physical therapy to strengthen the muscles around the spine
- Medications like NSAIDs to reduce pain and inflammation
- Epidural steroid injections for more severe cases
- Surgical options for cases that don’t respond to conservative treatment
It’s worth noting that surgery is usually considered a last resort. Most people find relief through a combination of lifestyle changes, physical therapy, and medication. But if your symptoms are severe and not improving, surgery might be an option worth exploring.
Physical Therapy: The Backbone of Treatment
Physical therapy is often one of the first lines of defense against DDD. A good physical therapist can help you strengthen the muscles around your spine, improve your flexibility, and reduce pain. They might use techniques like:
- Stretching exercises
- Core strengthening exercises
- Manual therapy to improve joint mobility
And the best part? Physical therapy is a proactive way to take control of your condition. It’s not just about treating the symptoms—it’s about addressing the root cause and building a stronger, healthier spine.
Living with Degenerative Disc Disease
Living with DDD doesn’t have to be a life sentence. While it’s true that there’s no cure for disc degeneration, there are plenty of ways to manage the condition and improve your quality of life. It’s all about finding the right strategies and making them a part of your daily routine.
Here are a few tips to help you live well with Degenerative Disc Disease:
- Maintain a healthy weight to reduce strain on your spine
- Practice good posture at all times
- Stay active with low-impact exercises like walking or swimming
- Avoid activities that put excessive strain on your back
It’s also important to listen to your body. If something feels off, don’t ignore it. And don’t be afraid to seek help when you need it. Whether it’s talking to your doctor, working with a physical therapist, or joining a support group, there are plenty of resources available to help you along the way.
Emotional Well-being and DDD
Let’s not forget about the emotional side of living with Degenerative Disc Disease. Chronic pain can take a toll on your mental health, leading to things like anxiety, depression, or feelings of isolation. That’s why it’s so important to prioritize your emotional well-being alongside your physical health.
Talking to a therapist or counselor can be a huge help, as can joining a support group where you can connect with others who understand what you’re going through. And don’t underestimate the power of self-care—things like mindfulness, meditation, or even just taking a few minutes each day to relax can make a big difference in how you feel.
Prevention and Long-Term Management
When it comes to Degenerative Disc Disease, prevention is key. While we can’t stop the aging process, there are plenty of things we can do to keep our spines healthy and strong. Here are a few tips:
- Exercise regularly to maintain muscle strength and flexibility
- Practice good posture in everyday activities
- Avoid smoking and limit alcohol consumption
- Eat a balanced diet rich in nutrients that support bone and joint health
And for those who already have DDD, long-term management is all about staying proactive. Regular check-ins with your healthcare provider, consistent physical therapy, and a commitment to healthy lifestyle choices can go a long way in keeping symptoms at bay.
The Role of Nutrition in Spine Health
Let’s talk about nutrition for a moment. What you eat can have a big impact on the health of your spine. Foods rich in calcium, vitamin D, and omega-3 fatty acids can help support strong bones and reduce inflammation. Think things like:
- Leafy green vegetables
- Fatty fish like salmon or sardines
- Nuts and seeds
- Fortified dairy products
On the flip side, try to limit processed foods, sugary snacks, and anything that can contribute to inflammation. Your spine will thank you!
Conclusion
Well, there you have it—a deep dive into Degenerative Disc Disease of the lumbar spine and its ICD 10 code. Whether you’re dealing with this condition yourself or just want to learn more, we hope this article has been helpful. Remember, knowledge is power, and understanding your diagnosis is the first step toward finding relief.
So what’s next? If you’re a patient, talk to your doctor about your symptoms and treatment options. If you’re a healthcare professional, keep educating yourself and your patients about the latest developments in DDD care. And don’t forget to share this article with anyone who might find it useful—spreading the word can make a big difference!
And hey, if you’ve got questions or
Article Recommendations
- Maligoshik Leaks Scandal Privacy Amp Public Reaction Exposed
- Movierulz Is Free Movie Streaming Safe Analysis Alternatives

Detail Author:
- Name : Ashton Gerhold
- Username : shaina.parisian
- Email : mkunze@deckow.info
- Birthdate : 1983-05-23
- Address : 463 Bernier Path Eliburgh, MS 75752-5946
- Phone : (863) 657-9447
- Company : Goldner-Kreiger
- Job : Tool Sharpener
- Bio : Quo eos earum fugit sed. Corrupti facere voluptatem vel nulla veritatis. Consequuntur pariatur sed ut ex in qui est iste. Sunt atque nobis qui molestiae. Et mollitia qui error libero iusto.
Socials
linkedin:
- url : https://linkedin.com/in/erling_id
- username : erling_id
- bio : Ut voluptas quaerat debitis delectus in.
- followers : 856
- following : 2143
instagram:
- url : https://instagram.com/edonnelly
- username : edonnelly
- bio : Magnam deleniti dolore sit expedita. Quia possimus consequatur repellendus. Ut a aliquam facere.
- followers : 878
- following : 238
twitter:
- url : https://twitter.com/erling_donnelly
- username : erling_donnelly
- bio : Iusto esse sed sunt unde in neque officiis. Est omnis quis rerum et voluptas sint. Maiores odit modi nihil blanditiis. Blanditiis aut ut natus omnis fuga.
- followers : 3029
- following : 1904
tiktok:
- url : https://tiktok.com/@edonnelly
- username : edonnelly
- bio : Assumenda nemo autem voluptatem magnam qui ex reiciendis.
- followers : 6393
- following : 1038